Exploring potential new patient benefits of allergy immunotherapy: Results from the REACT study
Beyond relevant outcomes in allergic rhinitis (AR) and asthma, the REACT (REAl world effeCtiveness of allergy immunoTherapy) study also revealed potential new findings related to allergy immunotherapy (AIT), such as reduced risk of pneumonia and hospitalisations.
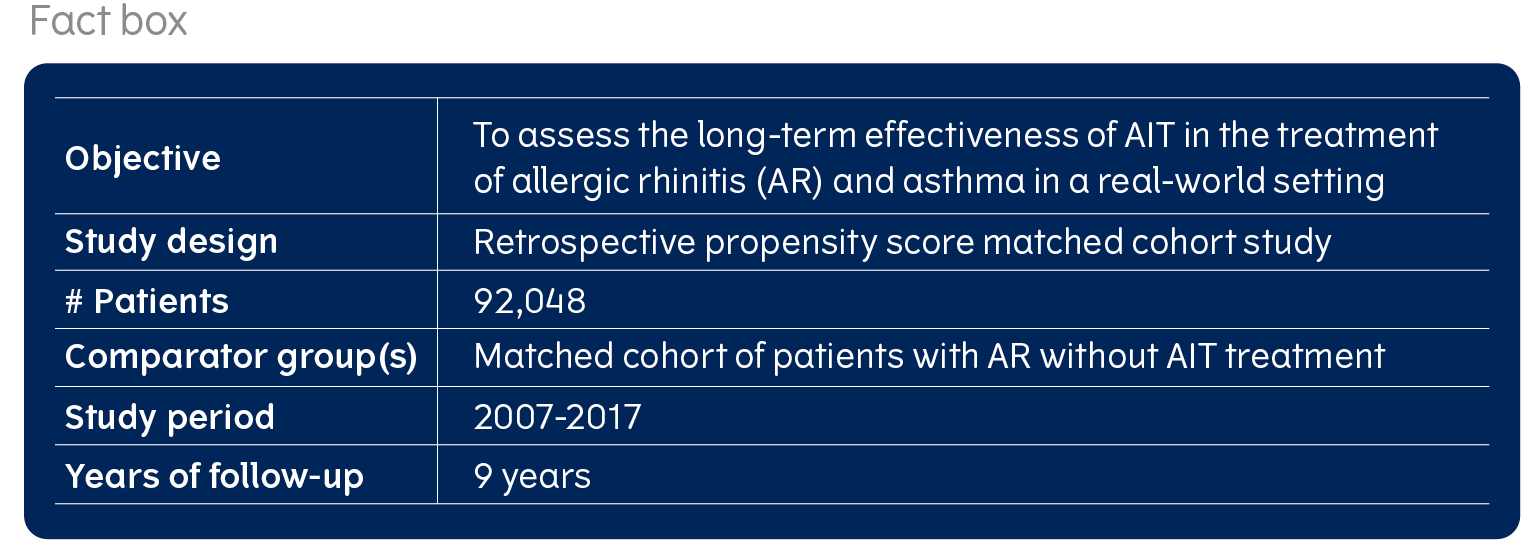
One of the key questions that the REACT study set out to answer, was whether there is evidence to support new hypotheses around the patient benefits of AIT. Therefore, as part of the pre-specified protocol, a set of exploratory outcomes, such as pneumonia (or lower respiratory tract infections), health care utilisation and costs, were defined.
The primary and secondary objectives of the study were to look at the impact of AIT on AR and asthma outcomes, read more here (link to long-term and asthma articles). The study design is described here.
AIT is associated with a reduced likelihood of pneumonia
The REACT st udy demonstrated an association between respiratory tract infections and AIT, as the likelihood of developing respiratory tract infections were lower for AIT-treated patients with pre-existing asthma versus those not treated with AIT. Additionally, the study also showed a reduced likelihood of antibiotic prescriptions related to pneumonia in the AIT group.
udy demonstrated an association between respiratory tract infections and AIT, as the likelihood of developing respiratory tract infections were lower for AIT-treated patients with pre-existing asthma versus those not treated with AIT. Additionally, the study also showed a reduced likelihood of antibiotic prescriptions related to pneumonia in the AIT group.
These results from the REACT study further substantiate a hypothesis which was initially generated by a recent which showed that patients with allergic asthma also have an increased risk of pneumonia, and hence allergy in asthma may be associated with a weaker immune response to fight of infections. The study further suggested that treatment with AIT had a protective effect against the risk of pneumonia.
In some cases, real world evidence can serve as a generator for hypotheses around novel clinical benefits which have not been investigated in a randomised, controlled trial (RCT)Such hypotheses need confirmation via an RCT to substantiate the evidence. Currently, a RCT is being conducted to assess the effect of house dust mite (HDM) sublingual AIT (SLIT)-tablets on antiviral immunity in patients with HDM-induced allergic asthma (VITAL study). The aim of this study is to expand understanding of the clinical significance of allergy in asthma in new ways and to assess the potential role of AIT in modulation of the immune response to prevent infections.
Read more about the VITAL study here.
Patients treated with AIT were less likely to have inpatient hospital stays and hospitalisations were shorter and less costly

The REACT study showed AIT is associated with a lower risk of hospitalisations (inpatient hospitalisations) across 9 years of follow-up, leading to fewer inpatient stays. This was shown for both patients with pre-existing asthma, but also for all patients with allergic rhinitis who had been treated with AIT. Not only did the AIT patients experience fewer inpatient stays, they also had shorter hospital stays leading to a lower cost for hospitalisations during the 9 years of follow up.
Patients suffering from allergic rhinitis often have related comorbidities, with asthma being the most prevalent. But eczema and conjunctivitis and even depression are also common comorbidities, increasing the burden of disease for patients and their use of health care resources. The REACT study shows that AIT has the potential to prevent some of that burden for both patients and health care systems.

Fritzsching B, et al.:” Long-term real-world effectiveness of allergy immunotherapy in patients with allergic rhinitis and asthma: results from the REACT study, a retrospective cohort study” Lancet Regional Health – Europe. 2021; https://doi.org/ 10.1016/j.lanepe.2021.100275