Improving asthma outcomes with allergy immunotherapy: Evidence from the REACT study
The REACT (REAl world effeCtiveness of allergy immunoTherapy) study demonstrated the long-term benefits of allergy immunotherapy (AIT) for patients with allergic rhinitis (AR) and pre-existing asthma, across several clinically relevant asthma outcomes.
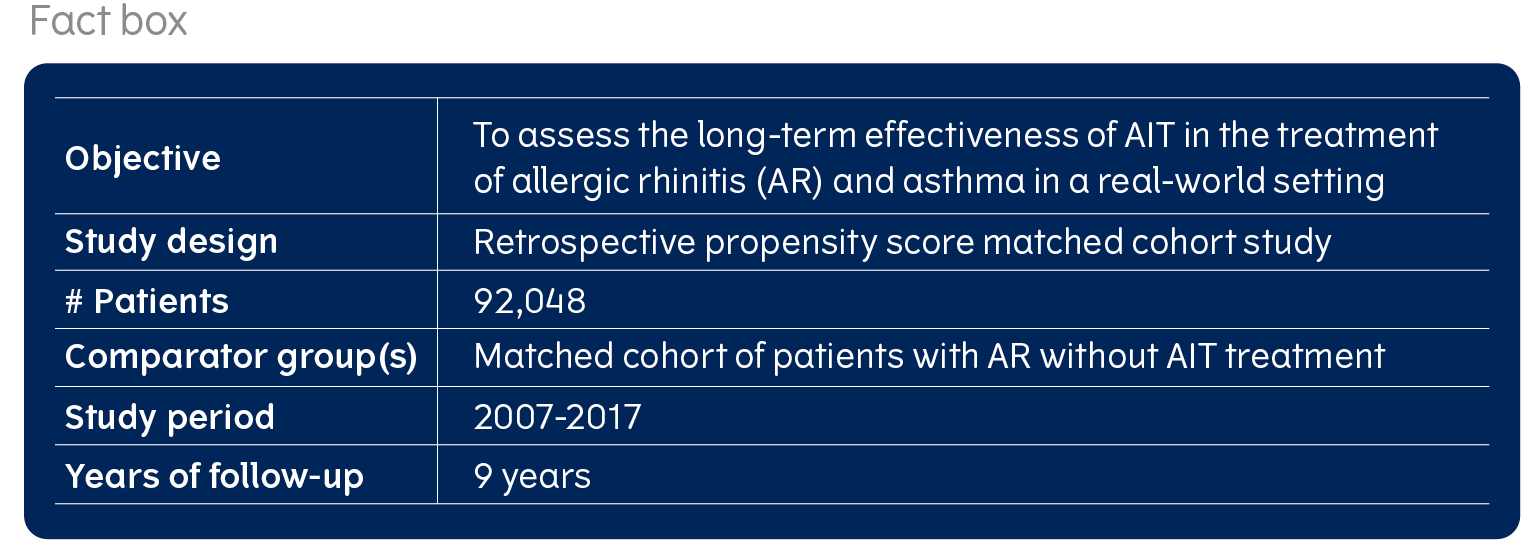
One of the key questions behind the REACT study, was whether AIT can lead to long-term, improved asthma control and the prevention of asthma exacerbations. Therefore, as a secondary objective, the study investigated the benefits of AIT for those patients with AR and concomitant asthma, in a sub-cohort of 29,228 patients with pre-existing asthma. Outcomes, such as asthma medication use, asthma treatment steps and asthma exacerbations were investigated. The study design is described here.
AIT is associated with long-term, sustained reductions in both controller and reliever asthma medications in AR patients with asthma

In the cohort of AR patients with pre-existing asthma, AIT was associated with greater reductions in asthma prescriptions over time compared to those not treated with AIT. The greater reductions in asthma prescriptions among AIT-treated patients were mainly for those having short-acting beta agonists (SABA) and inhaled corticosteroid (ICS)/long-acting beta agonist (LABA) prescriptions. As AIT was associated with reductions in both controller and reliever asthma medications, this points to the possibility of improved asthma control.
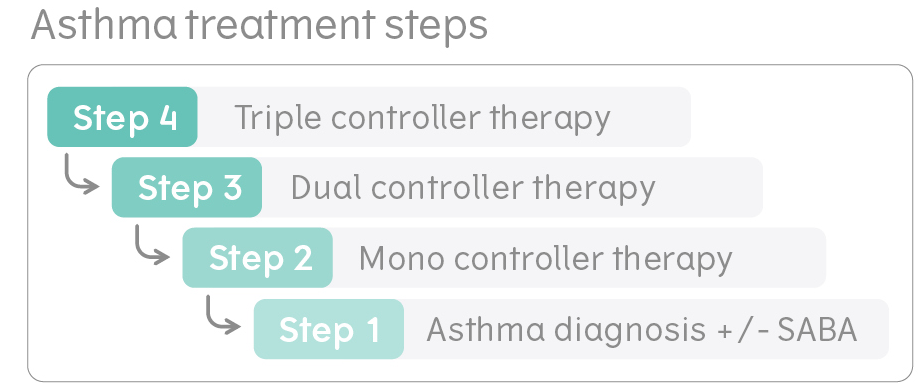
The greater reduction in both reliever and controller prescriptions for AIT-treated patients resulted in a significantly increased likelihood of a step down in their asthma treatment regimen. This might mean, for example, that a patient was able to step down from a dual therapy of ICS/LABA to a monotherapy of ICS only. The findings were sustained across the 9 years. Additionally, patients treated with AIT were not only more likely to step down, but also less likely to require a step up in their treatment.
AIT is associated with a reduced likelihood of experiencing severe asthma exacerbations

In addition to reducing asthma medication use and stepping down asthma treatment, AIT-treated patients in the pre-existing asthma cohort were also less likely to experience severe asthma exacerbations. In the AIT group, the likelihood of experiencing severe asthma exacerbations was lower across all 9 years of follow-up in this study, which may suggest that AIT can have a preventative effect on the risk of severe asthma exacerbations. Not only did the AIT group have a lower likelihood of exacerbations, but it also had fewer events across the years, compared to patients not treated with AIT.
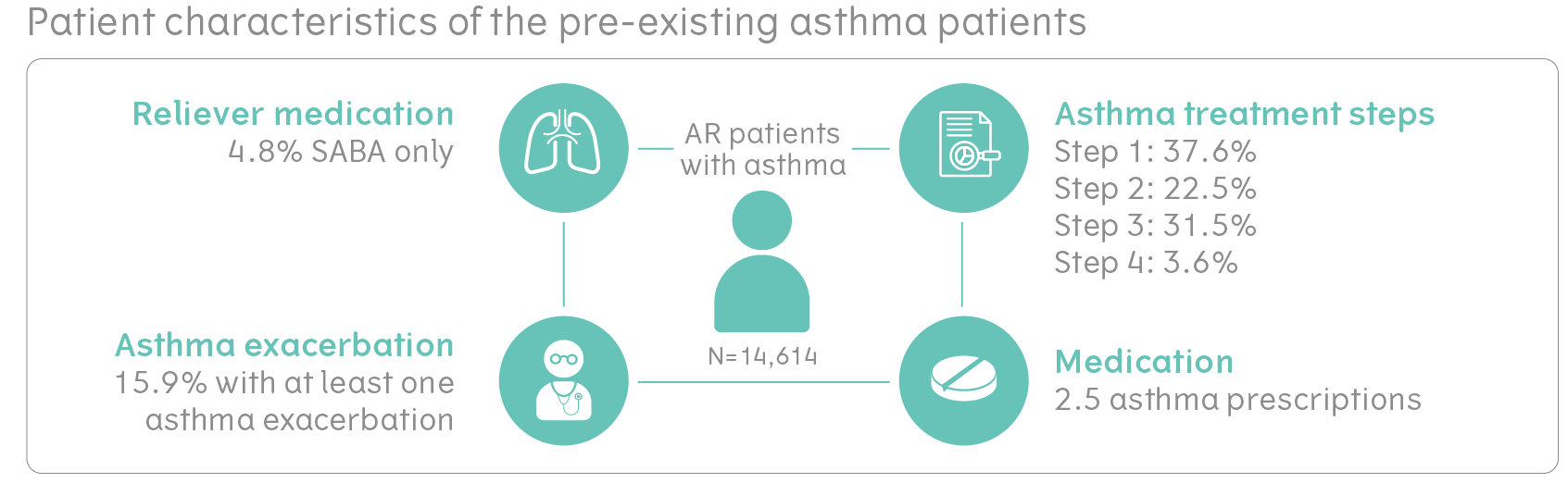
Patients with AR and pre-existing asthma in the REACT study
In total, 29,228 patients were included into the pre-existing asthma cohort based on an asthma diagnosis and/or 2 prescriptions of ICS/SABA in the year prior to AIT initiation. Patients with AR and pre-existing asthma and who had been treated with AIT were, on average, 28.3 years of age, and 53% of these patients were male. On average they had 2.5 asthma prescriptions in the year prior to starting AIT. Most were on asthma treatment steps 1-3, meaning that they were treated with either dual controller therapy (e.g., ICS/LABA), or monotherapy (e.g., ICS only), or had an asthma diagnosis with SABA use only. Furthermore, 15.9% had at least one severe asthma exacerbation in the year prior to AIT initiation. As the asthma cohort was matched via propensity score matching, the control group was similar on all these parameters.
More about the efficacy of AIT in asthma in RCTs
Click here

Fritzsching B, et al.:” Long-term real-world effectiveness of allergy immunotherapy in patients with allergic rhinitis and asthma: results from the REACT study, a retrospective cohort study” Lancet Regional Health – Europe. 2021; https://doi.org/ 10.1016/j.lanepe.2021.100275